Keratoconus, a condition where the cornea transforms into a cone shape, significantly affects vision, leading to a search for effective treatment.
Traditional treatments, including the use of rigid gas permeable and scleral contact lenses, have offered some relief, but not without challenges. Corneal transplant surgery, while beneficial for some, carries the risk of complications and doesn’t always halt the progression of the disease.
Enter the CREATE+CXL Protocol, a groundbreaking keratoconus surgery that combines topographic guided ablation with corneal collagen cross-linking. This innovative approach not only stops the progression but also corrects corneal unevenness, providing a substantial improvement in vision.
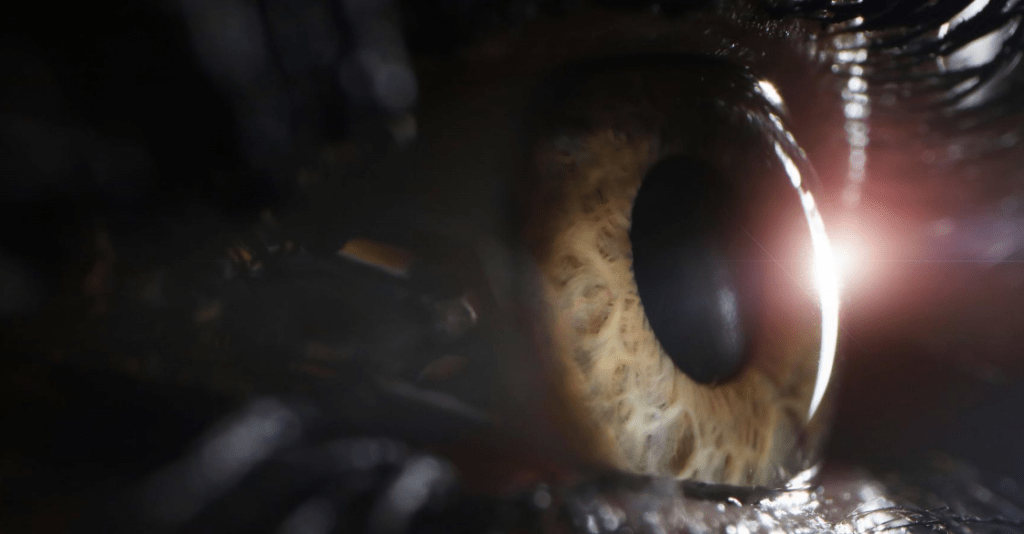
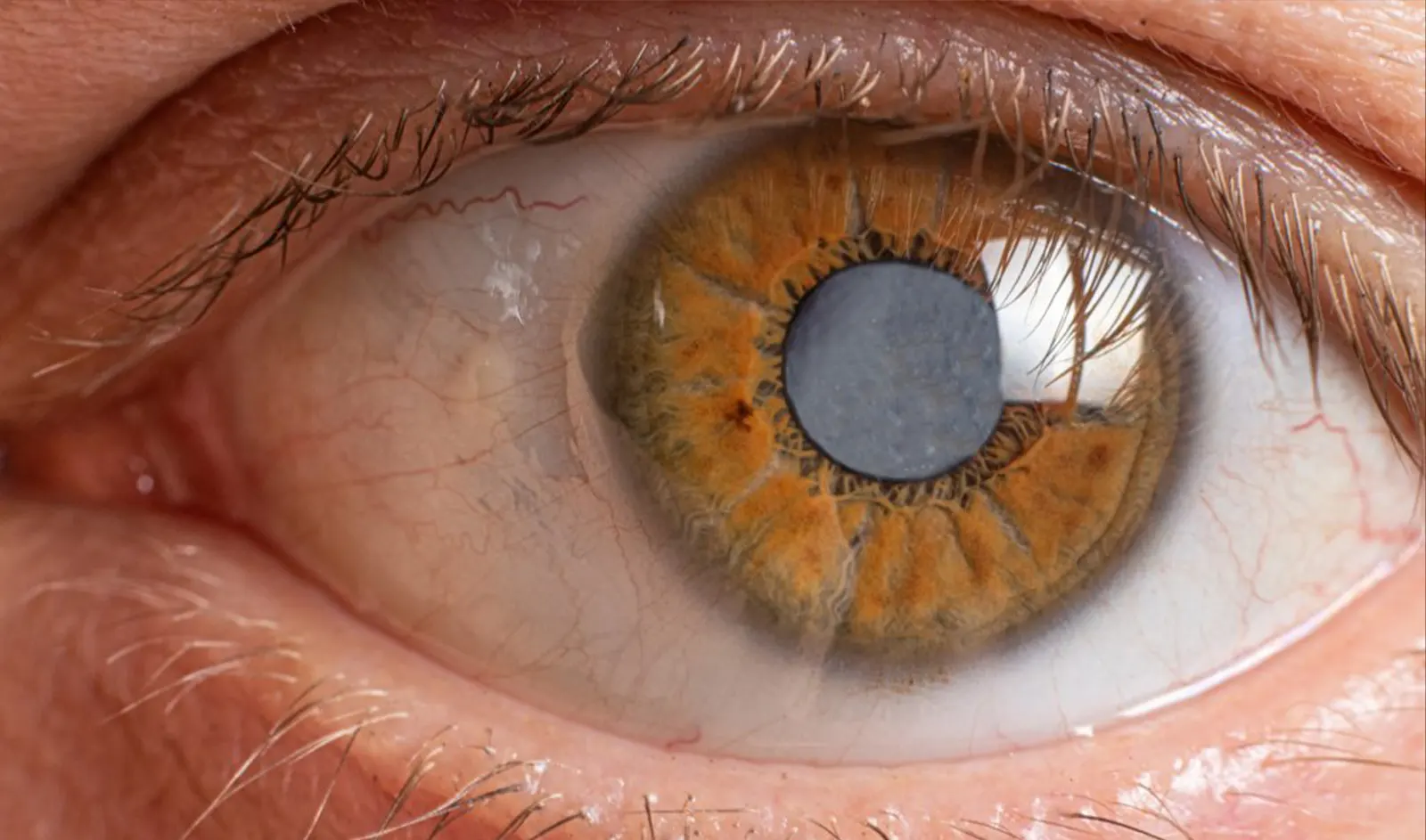
Before delving into the cutting-edge solutions offered by the CREATE+CXL Protocol, it’s essential to understand what keratoconus is and how it impacts those it affects. Keratoconus is an eye disorder that results in the progressive thinning and bulging of the cornea, the clear, dome-shaped surface that covers the front of the eye. This bulging transforms the cornea into a cone-like shape, distorting vision by altering the way light enters the eye.
Keratoconus typically manifests in the teenage years or early twenties and can progress at varying rates. Vision becomes increasingly blurred and distorted, making everyday tasks challenging. This condition is characterized by symptoms such as increased light sensitivity, glare, and halos around lights, significantly diminishing the quality of life for those affected.
Vision correction methods like rigid gas permeable contact lenses or scleral lenses have traditionally managed keratoconus, reshaping the cornea to improve vision.
For more advanced cases of keratoconus or when other methods fail to provide sufficient vision correction, doctors often consider corneal transplant surgery. However, these approaches, while effective to an extent, have their limitations and risks, highlighting the need for innovative treatment options.
This protocol marks a significant advancement in keratoconus treatment, offering a permanent solution that preserves the natural cornea. It’s an especially valuable option for those at risk of undergoing corneal transplant surgery, presenting a less invasive and more sustainable alternative.
Our clinic stands out for several reasons:
Living with keratoconus no longer means settling for blurred vision. The CREATE+CXL Protocol, among other modern treatments, opens up a world of clearer vision and improved quality of life for those affected by this condition. Our commitment goes beyond treating keratoconus; we aim to restore hope and clarity.
If you’re exploring options for keratoconus surgery, consider the innovative treatments we offer. Our team, including eye doctors specializing in advanced keratoconus, is ready to guide you towards clearer vision. Trust us to deliver the highest standard of care from the moment you request an appointment.
As keratoconus progresses, it can lead to blurred vision, increased sensitivity to light, glare, and the appearance of halos around lights, making daily tasks more challenging.
Glasses, soft contact lenses, rigid gas permeable (RGP) contact lenses, or scleral lenses have traditionally managed keratoconus to improve vision. In more advanced stages, doctors may consider corneal transplant surgery.
Yes, the CREATE+CXL Protocol aims to provide a permanent solution that preserves the patient’s natural cornea, setting it apart from traditional methods that might need ongoing adjustments or could result in complications.
Dr. Manoj Motwani is a renowned specialist in LASIK Laser Vision Correction and Reconstruction Repair, leading our clinic’s efforts in treating keratoconus with the CREATE+CXL Protocol. His expertise and innovative approach have helped many patients achieve clearer vision.
Our clinic stands out due to our expertise, innovation, and personalized care. We are pioneers in the CREATE+CXL Protocol, offering the latest in keratoconus treatment tailored to each patient’s specific needs and vision goals.
Keratoconus surgery has entered a new era with the CREATE+CXL Protocol, transforming how we treat keratoconus and other forms of corneal ectasia. By integrating topographic guided ablation with corneal collagen cross-linking, this protocol not only halts the disease’s progression but also offers a chance to improve vision significantly.
Whether you’re considering soft contact lenses, scleral contact lenses, or seeking a more permanent solution like the CREATE+CXL Protocol, our clinic is here to support your journey to clearer vision.
If you’re exploring keratoconus surgery options, you can request an appointment with us. Our team of specialists is ready to guide you towards a clearer vision. Trust us to provide the highest standard of care from your initial consultation through your treatment journey.
Cataract Surgery is the most performed surgical procedure in the United States, and has a phenomenal track record for improving…
Read More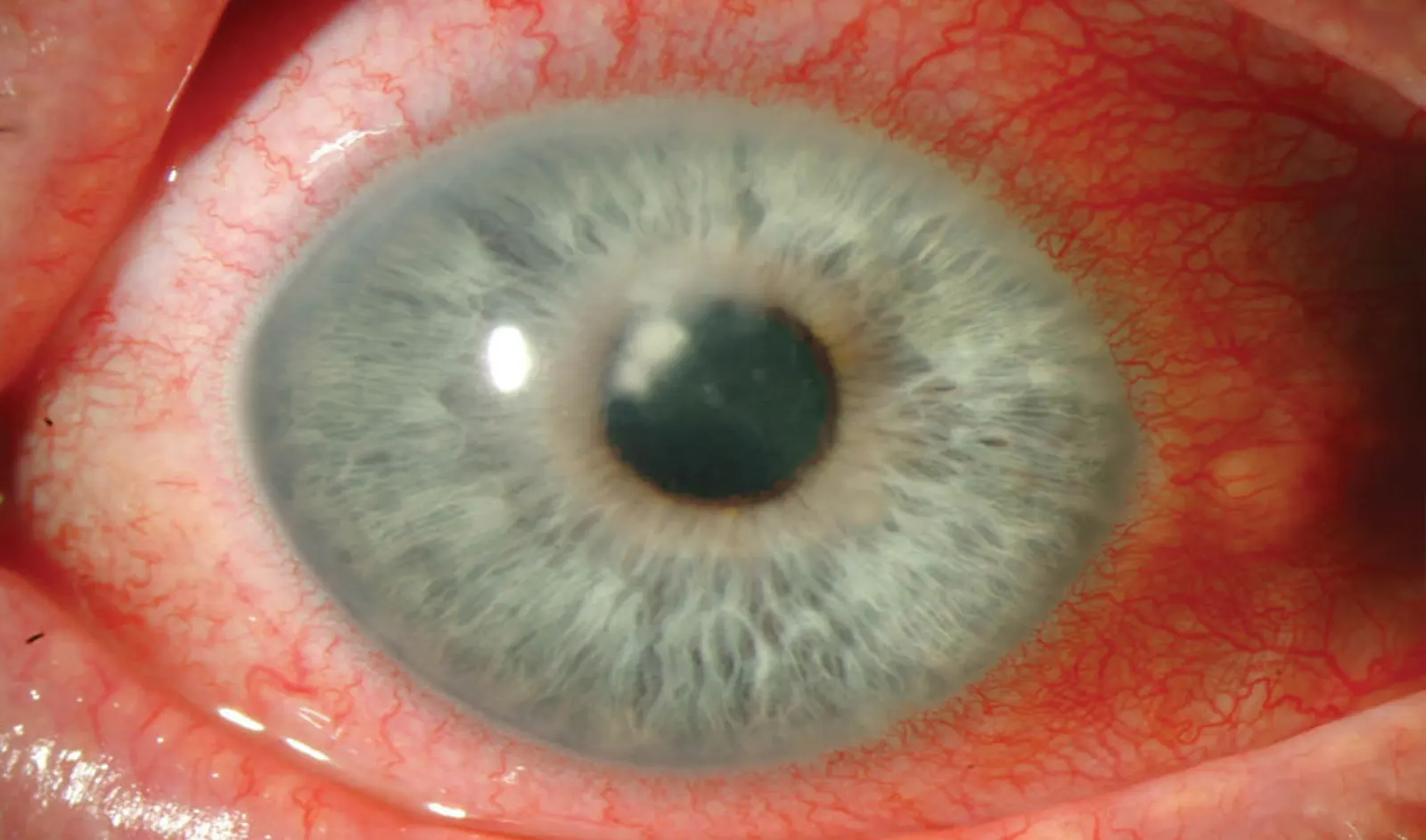
The treatment of trauma with topographic-guided ablation depends on the level of scarring caused by the trauma, the position of…
Read More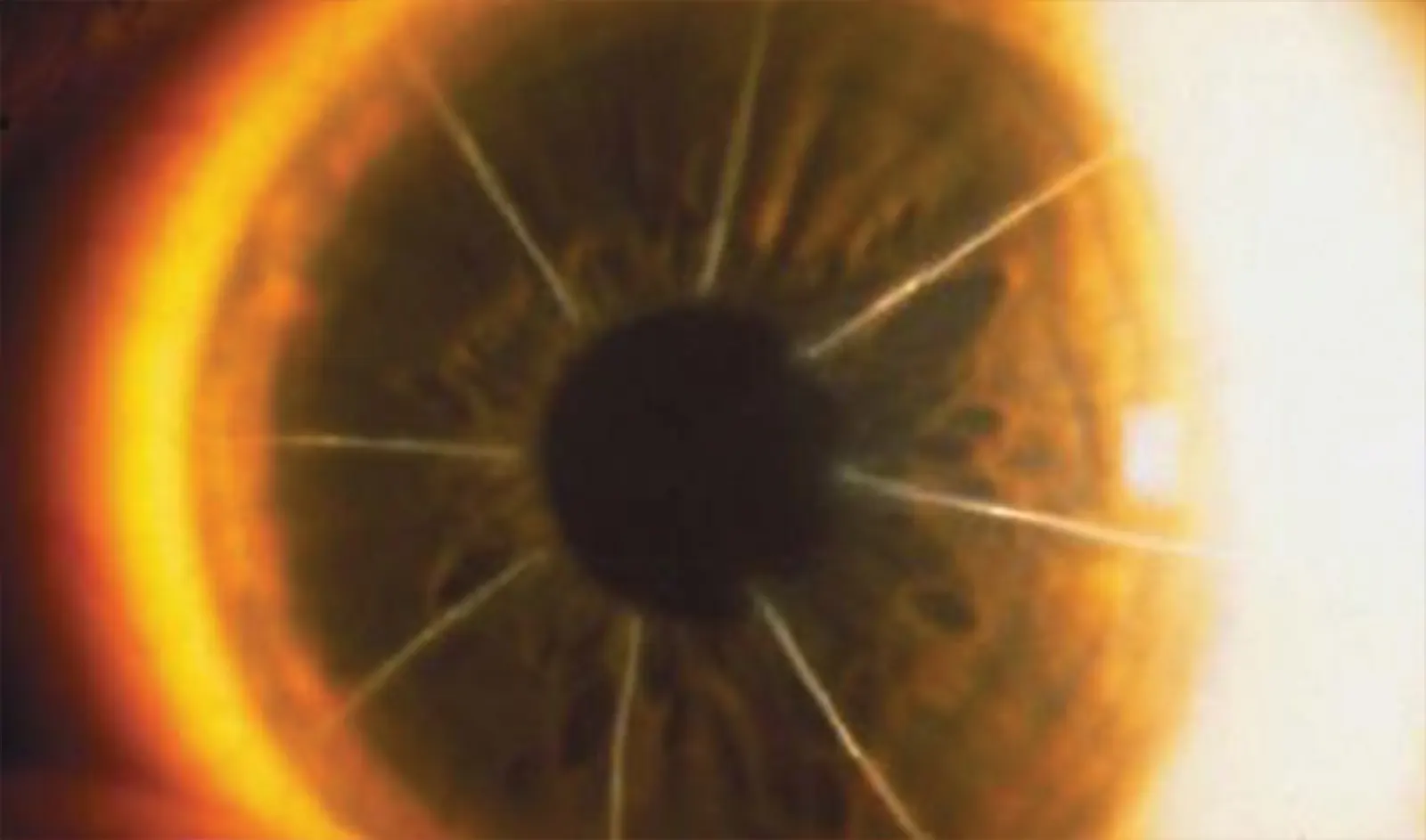
In the dynamic world of eye care, keratoconus treatment has become a focal point due to the condition’s impact on…
Read More